As a prevalent spinal condition, spinal stenosis is a significant cause of back pain among patients today. While most cases of spinal stenosis are resolved without surgery, some patients will require surgery to make a full recovery.
Thanks to advancing clinical technology, new spinal implants can be used to enhance surgical outcomes for stenosis patients. Here, we’ll discuss these implants and the role that they play in spinal stenosis surgery.
Spinal Stenosis: Explained
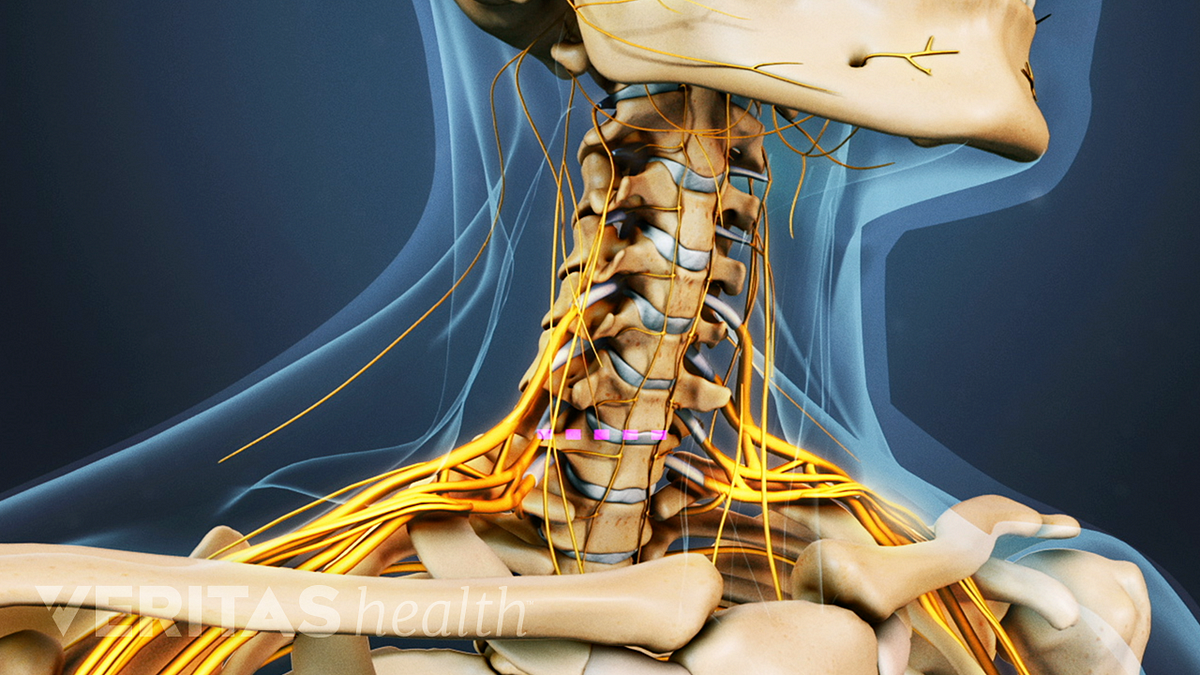
Spinal stenosis develops when the open space in the spinal canal decreases. As the spinal canal narrows, it may impinge on nearby nerves, leading to irritation, back pain, and neurological symptoms.
Dr. Lindsay Clark says that not all cases of spinal stenosis cause symptoms. Specifically, if the spinal canal becomes smaller, but doesn’t cause nerve impingement, the patient may not notice discomfort. However, if spinal nerves are compressed as a result of spinal stenosis, the following symptoms can occur:
- Back pain
- Neurological symptoms including weakness, numbness, and/or tingling in the extremities (for lumbar spinal stenosis, the legs; for cervical spinal stenosis, the arms)
- Sciatica (pain along the sciatic nerve, which extends from the lower back down the hips, buttocks, and legs)
Spinal stenosis can worsen over time if it’s not effectively treated. Severe cases of this spinal condition can lead to more serious symptoms including:
- Lost bladder/bowel control
- Severe pain and weakness in one or both legs
- Severe or gradually worsening numbness in the backs of the legs or inner thighs
Causes of Spinal Stenosis
There are several possible causes of spinal stenosis, the most common of which include:
Degenerative Disc Disease
Degenerative disc disease encompasses symptoms of back pain triggered by the gradual degeneration of a spinal disc. Caused mainly by the natural aging process, degenerative disc disease doesn’t always cause symptoms. However, it can trigger a range of spinal conditions, including spinal stenosis.
Herniated Disc
Whether due to degenerative disc disease, a spinal injury, or any number of other factors, a spinal disc exterior can weaken and develop a crack. The soft interior of the disc may then protrude from the crack, leading to disc herniation. The damaged disc may take up additional space in the spinal canal, causing spinal stenosis.
Osteoarthritis
Osteoarthritis is the most prevalent type of arthritis. It develops when the cartilage that protects the joints breaks down over time. If osteoarthritis affects the facet joints of the spine, the increased friction can stimulate the development of bone spurs.
Bone spurs are lumps of additional bone that can take up space in the spinal canal, leading to spinal stenosis.
Increased Thickness in The Spinal Ligaments
One of the spinal changes that can occur with the natural aging process is thickened ligaments. As the ligaments that connect the vertebrae become thicker with age, the space in the spinal canal decreases, potentially leading to spinal stenosis.
Treatment For Spinal Stenosis
As we’ve already mentioned, spinal stenosis is usually successfully managed with non-surgical methods, including:
- Physical therapy and spinal stenosis exercises, which strengthen the muscles that support the spine and promote proper spinal alignment
- Medications, which can help manage pain and inflammation from spinal stenosis
- Epidural steroid injections, which can help alleviate pain from spinal stenosis
- Alternative therapies such as massage and acupuncture for pain management
- Lifestyle adjustments, such as quitting smoking, sustaining a healthy body weight, and sticking to a low-impact exercise regimen
https://unsplash.com/photos/lrQPTQs7nQQ
When patients don’t respond to six months (or longer) of non-invasive treatment, spine specialists may recommend surgery.
What is Spinal Stenosis Surgery?
The goal of spinal stenosis surgery is to alleviate pressure on the impinged nerves by creating more space in the spinal canal. This is achieved through spinal decompression surgery.
Spinal decompression encompasses several different procedures that relieve compression on spinal nerves. The most commonly performed procedure for spinal stenosis is laminectomy, although foraminotomy and discectomy are also treatment options.
Laminectomy
In a laminectomy, the spinal surgeon removes some or all of the lamina of the affected vertebra(e). The lamina works like a roof, protecting the back of the spinal cord. Removing the lamina creates more space in the spinal canal and alleviates nerve impingement from spinal stenosis.
Spinal fusion is frequently performed along with spinal decompression to prevent spinal instability. The fusion process involves placing bone graft material between the affected vertebrae. Over time, the vertebrae will fuse into one bone.
https://www.pexels.com/photo/unrecognizable-crop-man-in-wristwatch-with-stethoscope-4021769/
Spinal Stenosis Surgery Implants
Implants are typically used in spinal stenosis surgery to provide stability and reinforcement. There are two key types of spinal implants: fusion implants and non-fusion implants.
- Fusion implants
Fusion implants assist in spinal fusion and are used along with bone graft material. The most widely-used fusion implants include cages, plates, and rods, which are typically fastened to the spinal bones with hooks and screws.
Unfortunately, spinal fusion limits patients’ back mobility. After fusion, patients lose the ability to bend, twist, and flex the spine at the fused segment. Additionally, spinal fusion can lead to degeneration of the adjacent segments, which is known as adjacent segment disease (ASD).
Alongside the risks and complications associated with spinal fusion, the recovery period for this type of spinal surgery is extensive, potentially taking up to a year.
- Non-fusion implants
A non-fusion spinal stenosis surgery implant is one of the most effective spinal fusion alternatives available. This type of spine device can dramatically decrease back surgery recovery time. Used along with laminectomy, a non-fusion implant can alleviate the patient’s pain without triggering complications.
Non-fusion implants don’t use bone graft material. Instead, devices like artificial discs replace damaged intervertebral disc material to retain the patient’s range of motion while stabilizing the spine.
If you’re suffering from spinal stenosis pain, talk to your doctor about the comprehensive range of treatment options available to you, including non-fusion implants.